Math Is Fun Forum
You are not logged in.
- Topics: Active | Unanswered
- Index
- » Science HQ
- » Placenta
Pages: 1
#1 2023-04-10 18:44:28
- Jai Ganesh
- Administrator

- Registered: 2005-06-28
- Posts: 53,057
Placenta
Placenta:
Gist
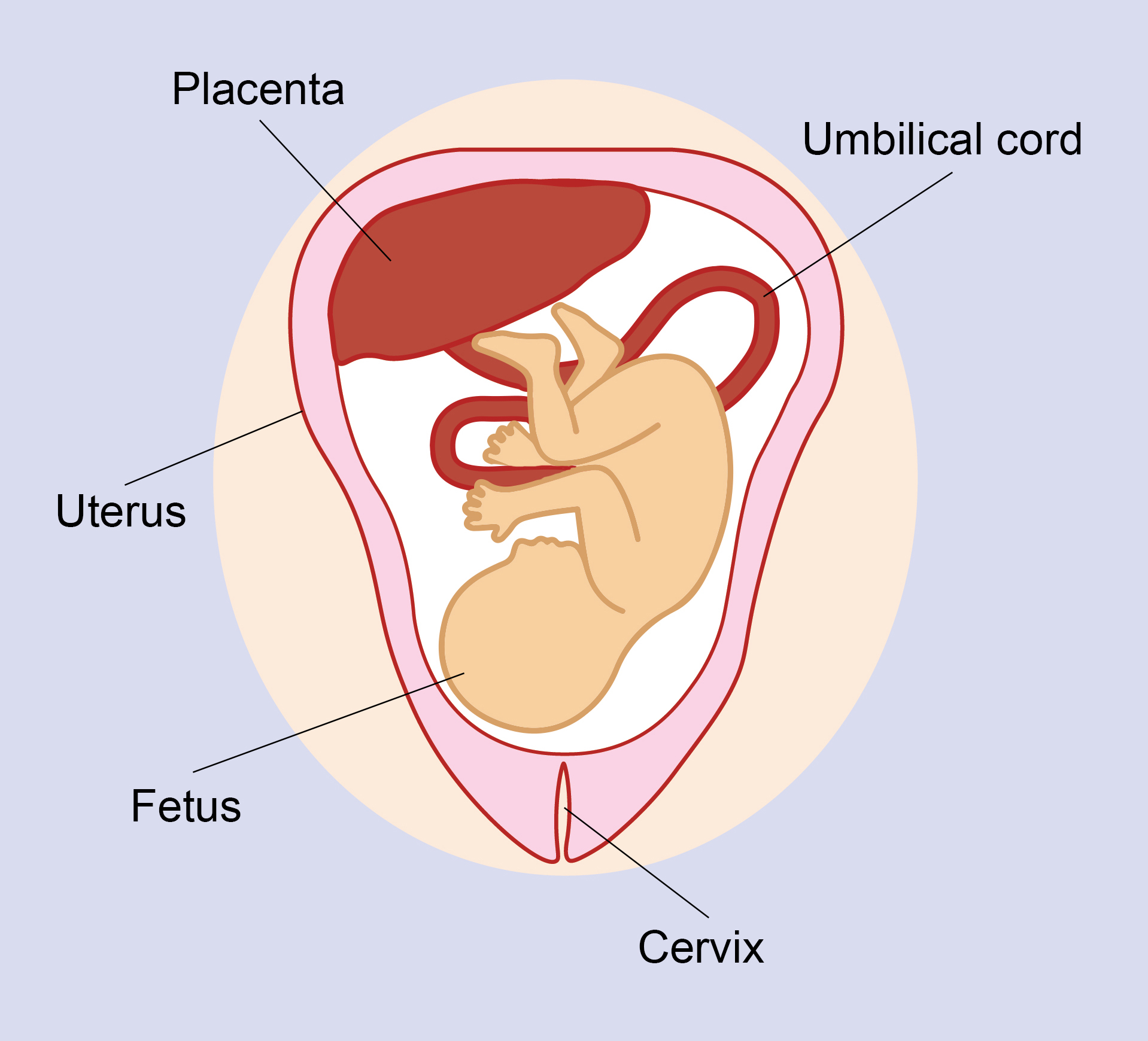
The placenta is an organ that develops in the uterus during pregnancy. This structure provides oxygen and nutrients to a growing baby. It also removes waste products from the baby's blood. The placenta attaches to the wall of the uterus, and the baby's umbilical cord arises from it.
Summary
Placenta, in zoology, is the vascular (supplied with blood vessels) organ in most mammals that unites the fetus to the uterus of the mother. It mediates the metabolic exchanges of the developing individual through an intimate association of embryonic tissues and of certain uterine tissues, serving the functions of nutrition, respiration, and excretion.
All of the fetal membranes function by adapting the developing fetus to the uterine environment. Lying in the chorionic cavity (a thin liquid-filled space) between two membranous envelopes (chorion and amnion) is a small balloon-like sac, yolk sac, or vitelline sac, attached by a delicate strand of tissue to the region where the umbilical cord (the structure connecting the fetus with the placenta) leaves the amnion. Two large arteries in the umbilical cord radiate from the attachment of the cord on the inner surface of the placenta and divide into small arteries that penetrate outward into the depths of the placenta through hundreds of branching and interlacing strands of tissue known as villi. The chorionic villi cause the mother’s blood vessels in their vicinity to rupture, and the villi become bathed directly in maternal blood. The constant circulation of fetal and maternal blood and the very thin tissue separation of fetal blood in the capillaries from maternal blood bathing the villi provide a mechanism for efficient interchange of blood constituents between the maternal and fetal bloodstreams without (normally) allowing any opportunity for the blood of one to pour across into the blood vessels of the other.
iNutrients, oxygen, and antibodies (proteins formed in response to a foreign substance, or antigen), as well as other materials in the mother’s blood, diffuse into the fetal blood in the capillaries of the villi, and nitrogenous wastes and carbon dioxide diffuse out of these capillaries into the maternal blood circulation. The purified and enriched blood in the capillaries of the villi is collected into fetal veins, which carry it back to the inner surface of the placenta and collect at the attachment of the cord to form the umbilical vein. This vein enters the cord alongside the two arteries and carries the blood back to the fetus, thus completing the circuit to and from the placenta.
Details
The placenta is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas and waste exchange between the physically separate maternal and fetal circulations, and is an important endocrine organ, producing hormones that regulate both maternal and fetal physiology during pregnancy. The placenta connects to the fetus via the umbilical cord, and on the opposite aspect to the maternal uterus in a species-dependent manner. In humans, a thin layer of maternal decidual (endometrial) tissue comes away with the placenta when it is expelled from the uterus following birth (sometimes incorrectly referred to as the 'maternal part' of the placenta). Placentas are a defining characteristic of placental mammals, but are also found in marsupials and some non-mammals with varying levels of development.
Mammalian placentas probably first evolved about 150 million to 200 million years ago. The protein syncytin, found in the outer barrier of the placenta (the syncytiotrophoblast) between mother and fetus, has a certain RNA signature in its genome that has led to the hypothesis that it originated from an ancient retrovirus: essentially a virus that helped pave the transition from egg-laying to live-birth.
The word placenta comes from the Latin word for a type of cake, from Greek "flat, slab-like", with reference to its round, flat appearance in humans. The classical plural is placentae, but the form placentas is more common in modern English.
Evolution and phylogenetic diversity
The placenta has evolved independently multiple times, probably starting in fish, where it originated multiple times, including the genus Poeciliopsis. Placentation has also evolved in some reptiles.
The mammalian placenta evolved more than 100 million years ago and was a critical factor in the explosive diversification of placental mammals. Although all mammalian placentas have the same functions, there are important differences in structure and function in different groups of mammals. For example, human, bovine, equine and canine placentas are very different at both the gross and the microscopic levels. Placentas of these species also differ in their ability to provide maternal immunoglobulins to the fetus.
Structure
Placental mammals, including humans, have a chorioallantoic placenta that forms from the chorion and allantois. In humans, the placenta averages 22 cm (9 inch) in length and 2–2.5 cm (0.8–1 inch) in thickness, with the center being the thickest, and the edges being the thinnest. It typically weighs approximately 500 grams (just over 1 lb). It has a dark reddish-blue or crimson color. It connects to the fetus by an umbilical cord of approximately 55–60 cm (22–24 inch) in length, which contains two umbilical arteries and one umbilical vein. The umbilical cord inserts into the chorionic plate (has an eccentric attachment). Vessels branch out over the surface of the placenta and further divide to form a network covered by a thin layer of cells. This results in the formation of villous tree structures. On the maternal side, these villous tree structures are grouped into lobules called cotyledons. In humans, the placenta usually has a disc shape, but size varies vastly between different mammalian species.
The placenta occasionally takes a form in which it comprises several distinct parts connected by blood vessels. The parts, called lobes, may number two, three, four, or more. Such placentas are described as bilobed/bilobular/bipartite, trilobed/trilobular/tripartite, and so on. If there is a clearly discernible main lobe and auxiliary lobe, the latter is called a succenturiate placenta. Sometimes the blood vessels connecting the lobes get in the way of fetal presentation during labor, which is called vasa previa.
Gene and protein expression
About 20,000 protein coding genes are expressed in human cells and 70% of these genes are expressed in the normal mature placenta. Some 350 of these genes are more specifically expressed in the placenta and fewer than 100 genes are highly placenta specific. The corresponding specific proteins are mainly expressed in trophoblasts and have functions related to pregnancy. Examples of proteins with elevated expression in placenta compared to other organs and tissues are PEG10 and the cancer testis antigen PAGE4 and expressed in cytotrophoblasts, CSH1 and KISS1 expressed in syncytiotrophoblasts, and PAPPA2 and PRG2 expressed in extravillous trophoblasts.
Physiology:
Development
The placenta begins to develop upon implantation of the blastocyst into the maternal endometrium, very early on in pregnancy at about week 4.
The outer layer of the late blastocyst, is formed of trophoblasts, cells that form the outer layer of the placenta. This outer layer is divided into two further layers: the underlying cytotrophoblast layer and the overlying syncytiotrophoblast layer. The syncytiotrophoblast is a multinucleated continuous cell layer that covers the surface of the placenta. It forms as a result of differentiation and fusion of the underlying cytotrophoblasts, a process that continues throughout placental development. The syncytiotrophoblast contributes to the barrier function of the placenta.
The placenta grows throughout pregnancy. Development of the maternal blood supply to the placenta is complete by the end of the first trimester of pregnancy week 14 (DM).
Placental circulation
Maternal blood fills the intervillous space, nutrients, water, and gases are actively and passively exchanged, then deoxygenated blood is displaced by the next maternal pulse.
Maternal placental circulation
In preparation for implantation of the blastocyst, the endometrium undergoes decidualization. Spiral arteries in the decidua are remodeled so that they become less convoluted and their diameter is increased. The increased diameter and straighter flow path both act to increase maternal blood flow to the placenta. There is relatively high pressure as the maternal blood fills intervillous space through these spiral arteries which bathe the fetal villi in blood, allowing an exchange of gases to take place. In humans and other hemochorial placentals, the maternal blood comes into direct contact with the fetal chorion, though no fluid is exchanged. As the pressure decreases between pulses, the deoxygenated blood flows back through the endometrial veins.
Maternal blood flow begins between days 5–12, and is approximately 600–700 ml/min at term.
Fetoplacental circulation
Deoxygenated fetal blood passes through umbilical arteries to the placenta. At the junction of umbilical cord and placenta, the umbilical arteries branch radially to form chorionic arteries. Chorionic arteries, in turn, branch into cotyledon arteries. In the villi, these vessels eventually branch to form an extensive arterio-capillary-venous system, bringing the fetal blood extremely close to the maternal blood; but no intermingling of fetal and maternal blood occurs ("placental barrier").
Endothelin and prostanoids cause vasoconstriction in placental arteries, while nitric oxide causes vasodilation. On the other hand, there is no neural vascular regulation, and catecholamines have only little effect.
The fetoplacental circulation is vulnerable to persistent hypoxia or intermittent hypoxia and reoxygenation, which can lead to generation of excessive free radicals. This may contribute to pre-eclampsia and other pregnancy complications. It is proposed that melatonin plays a role as an antioxidant in the placenta.
This begins at day 17–22.
Birth
Placental expulsion begins as a physiological separation from the wall of the uterus. The period from just after the child is born until just after the placenta is expelled is called the "third stage of labor". The placenta is usually expelled within 15–30 minutes of birth.
Placental expulsion can be managed actively, for example by giving oxytocin via intramuscular injection followed by cord traction to assist in delivering the placenta. Alternatively, it can be managed expectantly, allowing the placenta to be expelled without medical assistance. Blood loss and the risk of postpartum bleeding may be reduced in women offered active management of the third stage of labour, however there may be adverse effects and more research is necessary.
The habit is to cut the cord immediately after birth, but it is theorised that there is no medical reason to do this; on the contrary, it is theorised that not cutting the cord helps the baby in its adaptation to extrauterine life, especially in preterm infants.
Microbiome
The placenta is traditionally thought to be sterile, but recent research suggests that a resident, non-pathogenic, and diverse population of microorganisms may be present in healthy tissue. However, whether these microbes exist or are clinically important is highly controversial and is the subject of active research.
It appears to me that if one wants to make progress in mathematics, one should study the masters and not the pupils. - Niels Henrik Abel.
Nothing is better than reading and gaining more and more knowledge - Stephen William Hawking.
Offline
Pages: 1
- Index
- » Science HQ
- » Placenta