Math Is Fun Forum
You are not logged in.
- Topics: Active | Unanswered
- Index
- » Science HQ
- » Thyroid
Pages: 1
#1 2025-05-07 00:22:37
- Jai Ganesh
- Administrator

- Registered: 2005-06-28
- Posts: 53,341
Thyroid
Thyroid
Gist
The thyroid is a butterfly-shaped gland in the front of your neck that produces hormones regulating energy use in your body. These hormones affect nearly every organ and function, including breathing, heart rate, weight, digestion, and mood. The thyroid gland is an endocrine gland, meaning it produces and releases hormones
Your thyroid is an important endocrine gland that makes and releases certain hormones. Your thyroid's main job is to control your metabolism — how your body uses energy. Sometimes, your thyroid doesn't work properly. These conditions are common and treatable.
Summary
The thyroid, or thyroid gland, is an endocrine gland in vertebrates. In humans, it is a butterfly-shaped gland located in the neck below the Adam's apple. It consists of two connected lobes. The lower two thirds of the lobes are connected by a thin band of tissue called the isthmus (pl.: isthmi). Microscopically, the functional unit of the thyroid gland is the spherical thyroid follicle, lined with follicular cells (thyrocytes), and occasional parafollicular cells that surround a lumen containing colloid.
The thyroid gland secretes three hormones: the two thyroid hormones – triiodothyronine (T3) and thyroxine (T4) – and a peptide hormone, calcitonin. The thyroid hormones influence the metabolic rate and protein synthesis and growth and development in children. Calcitonin plays a role in calcium homeostasis.
Secretion of the two thyroid hormones is regulated by thyroid-stimulating hormone (TSH), which is secreted from the anterior pituitary gland. TSH is regulated by thyrotropin-releasing hormone (TRH), which is produced by the hypothalamus.
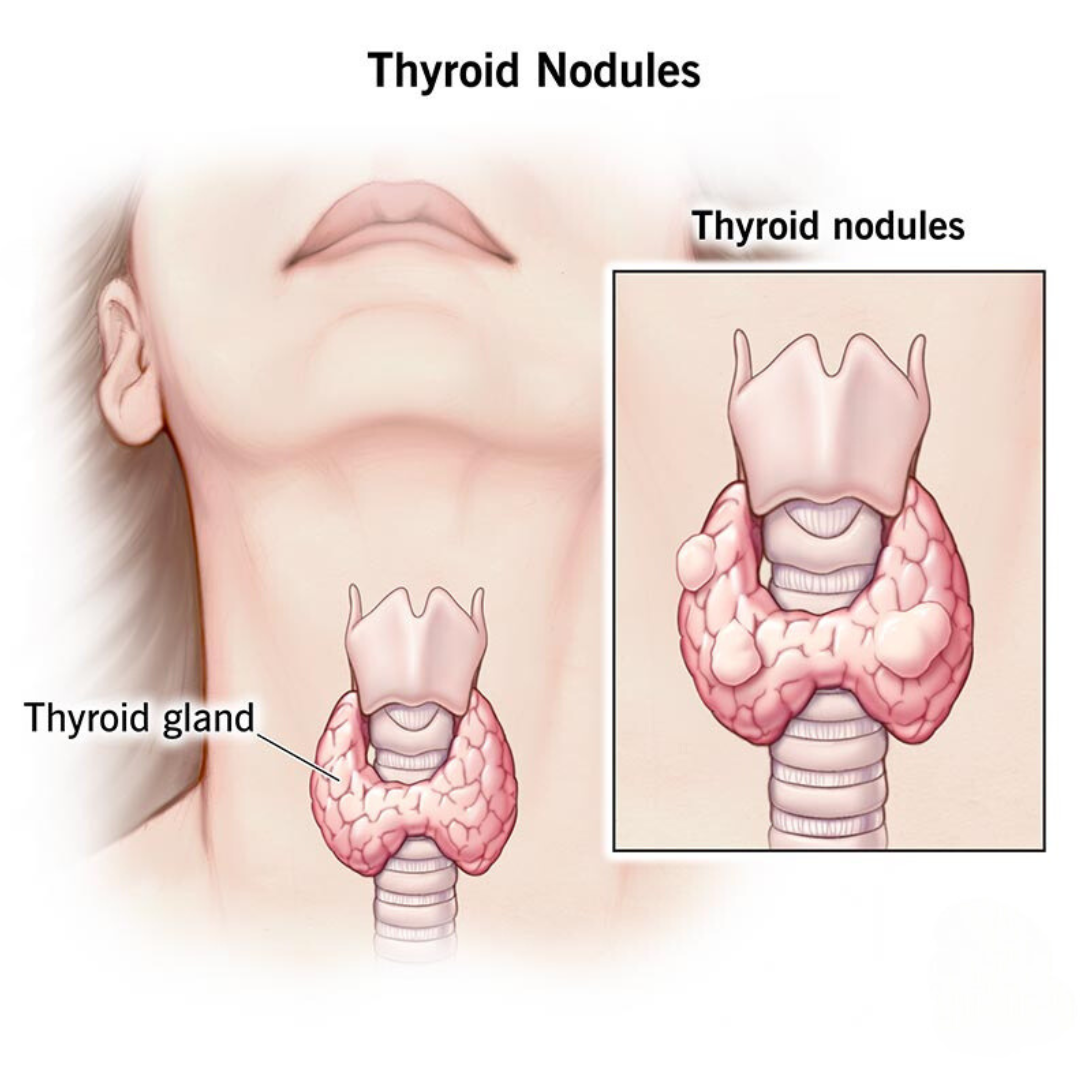
Thyroid disorders include hyperthyroidism, hypothyroidism, thyroid inflammation (thyroiditis), thyroid enlargement (goitre), thyroid nodules, and thyroid cancer. Hyperthyroidism is characterized by excessive secretion of thyroid hormones: the most common cause is the autoimmune disorder Graves' disease. Hypothyroidism is characterized by a deficient secretion of thyroid hormones: the most common cause is iodine deficiency. In iodine-deficient regions, hypothyroidism (due to iodine deficiency) is the leading cause of preventable intellectual disability in children. In iodine-sufficient regions, the most common cause of hypothyroidism is the autoimmune disorder Hashimoto's thyroiditis.
Details
Thyroid gland is an endocrine gland that is located in the anterior part of the lower neck, below the larynx (voice box). The thyroid secretes hormones vital to metabolism and growth. Any enlargement of the thyroid, regardless of cause, is called a goitre.
Anatomy of the thyroid gland
The thyroid arises from a downward outpouching of the floor of the pharynx, and a persisting remnant of this migration is known as a thyroglossal duct. The gland itself consists of two oblong lobes lying on either side of the trachea (windpipe) and connected by a narrow band of tissue called the isthmus. In normal adults the thyroid gland weighs 10 to 15 grams (0.4 to 0.5 ounce), though it has the capacity to grow much larger.
The lobes of the gland, as well as the isthmus, contain many small globular sacs called follicles. The follicles are lined with follicular cells and are filled with a fluid known as colloid that contains the prohormone thyroglobulin. The follicular cells contain the enzymes needed to synthesize thyroglobulin, as well as the enzymes needed to release thyroid hormone from thyroglobulin. When thyroid hormones are needed, thyroglobulin is reabsorbed from the colloid in the follicular lumen into the cells, where it is split into its component parts, including the two thyroid hormones thyroxine (T4) and triiodothyronine (T3). The hormones are then released, passing from the cells into the circulation.
Biochemistry of thyroid hormone
Thyroxine and triiodothyronine contain iodine and are formed from thyronines, which are composed of two molecules of the amino acid tyrosine. (Both iodine and tyrosine are acquired in the diet.) Thyroxine contains four iodine atoms, and triiodothyronine contains three iodine atoms. Because each molecule of tyrosine binds one or two iodine atoms, two tyrosines are used to synthesize both thyroxine and triiodothyronine. These two hormones are the only biologically active substances that contain iodine, and they cannot be produced in the absence of iodine. The process leading to the eventual synthesis of thyroxine and triiodothyronine begins in the thyroid follicular cells, which concentrate iodine from the serum. The iodine is then oxidized and attached to tyrosine residues (forming compounds called iodotyrosines) within thyroglobulin molecules. The iodinated tyrosine residues are then rearranged to form thyroxine and triiodothyronine. Therefore, thyroglobulin serves not only as the structure within which thyroxine and triiodothyronine are synthesized but also as the storage form of the two hormones.
Considerably more thyroxine is produced and secreted by the thyroid gland than is triiodothyronine. However, thyroxine is converted to triiodothyronine in many tissues by the action of enzymes called deiodinases. After thyroxine enters a cell, deiodinases located in the cytoplasm remove one of its four iodine atoms, converting it into triiodothyronine. The triiodothyronine either enters the nucleus of the cell or is returned to the circulation. As a result, all of the thyroxine and about 20 percent of the triiodothyronine produced each day come from the thyroid gland. The remaining 80 percent of triiodothyronine comes from deiodination of thyroxine outside of the thyroid. Most if not all of the action of thyroid hormone in its target tissues is exerted by triiodothyronine. Therefore, thyroxine may be considered a circulating precursor of triiodothyronine.
In serum more than 99 percent of the thyroxine and triiodothyronine is bound to one of three proteins. These binding proteins are known as thyroxine-binding globulin, transthyretin (thyroxine-binding prealbumin), and albumin. The remaining thyroxine and triiodothyronine (less than 1 percent) is free, or unbound. When free hormone enters a cell, it is replenished immediately by hormone attached to the binding proteins. The binding proteins serve as reservoirs of the two hormones to protect the tissues from sudden surges of thyroid hormone production and probably also to facilitate delivery of the hormones to the cells of large, solid organs such as the liver.
Essentially all cells in the body are target cells of triiodothyronine. Once triiodothyronine is inside a cell, it enters the nucleus, where it binds to proteins known as nuclear receptors. The triiodothyronine-receptor complexes then bind to deoxyribonucleic acid (DNA) molecules. This results in an increase in the rate at which the affected DNA molecules are transcribed to produce messenger ribonucleic acid (mRNA) molecules and an increase in the rate of synthesis of the protein (translation) coded for by the DNA (by way of the mRNA). Triiodothyronine increases the transcription of DNA molecules that code for many different proteins; however, it also inhibits the transcription of DNA that codes for certain other proteins. The patterns of activation and inhibition differ in different tissue and cell types.
Actions of thyroid hormone
The substances produced in increased quantities in response to triiodothyronine secretion include many enzymes, cell constituents, and hormones. Key among them are proteins that regulate the utilization of nutrients and the consumption of oxygen by the mitochondria of cells. Mitochondria are the sites at which energy is produced in the form of adenosine triphosphate (ATP) or is dissipated in the form of heat. Triiodothyronine activates substances that increase the proportion of energy that is dissipated as heat. It also stimulates carbohydrate utilization, lipid production and metabolism (thereby increasing cholesterol utilization), and central and autonomic nervous system activation, resulting in increased contraction of cardiac muscle and increased heart rate. During fetal life and in infancy this stimulatory activity of triiodothyronine is critically important for normal neural and skeletal growth and development; in both the unborn and the newborn, thyroid deficiency is associated with dwarfism and intellectual disability.
Regulation of thyroid hormone secretion
The thyroid gland is one component of the hypothalamic-pituitary-thyroid axis, which is a prime example of a negative feedback control system. The production and secretion of thyroxine and triiodothyronine by the thyroid gland are stimulated by the hypothalamic hormone thyrotropin-releasing hormone and the anterior pituitary hormone thyrotropin. In turn, the thyroid hormones inhibit the production and secretion of both thyrotropin-releasing hormone and thyrotropin. Decreased production of thyroid hormone results in increased thyrotropin secretion and thus increased thyroid hormone secretion. This restores serum thyroid hormone concentrations to normal levels (if the thyroid gland is not severely damaged). Conversely, increased production of thyroid hormone or administration of high doses of thyroid hormone inhibit the secretion of thyrotropin. As a result of this inhibition, serum thyroid hormone concentrations are able to fall toward normal levels. The complex interactions between thyroid hormone and thyrotropin maintain serum thyroid hormone concentrations within narrow limits. However, if the thyroid gland is severely damaged or if there is excessive thyroid hormone production independent of thyrotropin stimulation, hypothyroidism (thyroid deficiency) or hyperthyroidism (thyroid excess) ensues.
As noted above, much of the triiodothyronine produced each day is produced by deiodination of thyroxine in extrathyroidal tissues. The conversion of thyroxine to triiodothyronine significantly decreases in response to many adverse conditions, such as malnutrition, injury, or illness (including infections, cancer, and liver, heart, and kidney diseases). The production of triiodothyronine is also inhibited by starvation and by several drugs, notably amiodarone, a drug used to treat patients with cardiac rhythm disorders. In each of these situations, serum and tissue triiodothyronine concentrations decrease. This decrease in triiodothyronine production may be a beneficial adaptation to starvation and illness because it reduces the breakdown of protein and slows the use of nutrients for generating heat, thereby maintaining tissue integrity and conserving energy resources.
The fetal thyroid gland begins to function at about 12 weeks of gestation, and its function increases progressively thereafter. Within minutes after birth there is a sudden surge in thyrotropin secretion, followed by a marked increase in serum thyroxine and triiodothyronine concentrations. The concentrations of thyroid hormones then gradually decline, reaching adult values at the time of puberty. Thyroid hormone secretion increases in pregnant women. Therefore, women with thyroid deficiency who become pregnant usually need higher doses of thyroid hormone than when they are not pregnant. There is little change in thyroid secretion in older adults as compared with younger adults.
The thyroid gland and calcitonin
The C cells, or parafollicular cells, of the thyroid gland (indicated by the arrow marked “P”) produce a hormone called calcitonin, which regulates serum calcium levels.
The thyroid gland is also the site of the production of calcitonin, a hormone that can lower serum calcium concentrations. The cells that produce calcitonin, which are called C cells, or parafollicular cells arise, separately from the thyroid and migrate into it during development of the embryo. The C cells end up nestled in the spaces between the follicles. Because these cells have a separate embryological origin from the thyroid follicular cells,and because they secrete calcitonin, they in essence form a separate endocrine organ. (In some animals the C cells remain separate from the thyroid.)
Calcitonin is secreted in response to high serum calcium concentrations, and it lowers the concentrations acutely by inhibiting the resorption of bone. However, its action wanes within days, so calcitonin therapy is not an effective treatment for high calcium levels.
Diseases of the thyroid gland
The most common thyroid disease is thyroid nodular disease (the appearance of small, usually benign lumps within an otherwise healthy gland), followed by hypothyroidism, hyperthyroidism, and thyroid cancer.
Additional Information
Your thyroid is a small, butterfly-shaped gland located at the front of your neck under your skin. It’s a part of your endocrine system and controls many of your body’s important functions by producing and releasing (secreting) certain hormones. Your thyroid’s main job is to control the speed of your metabolism (metabolic rate), which is the process of how your body transforms the food you consume into energy. All of the cells in your body need energy to function.
When your thyroid isn’t working properly, it can impact your entire body.
It appears to me that if one wants to make progress in mathematics, one should study the masters and not the pupils. - Niels Henrik Abel.
Nothing is better than reading and gaining more and more knowledge - Stephen William Hawking.
Offline
Pages: 1
- Index
- » Science HQ
- » Thyroid