Math Is Fun Forum
You are not logged in.
- Topics: Active | Unanswered
Pages: 1
#1 2024-09-17 15:45:52
- Jai Ganesh
- Administrator

- Registered: 2005-06-28
- Posts: 52,752
Dura mater
Dura mater
Gist
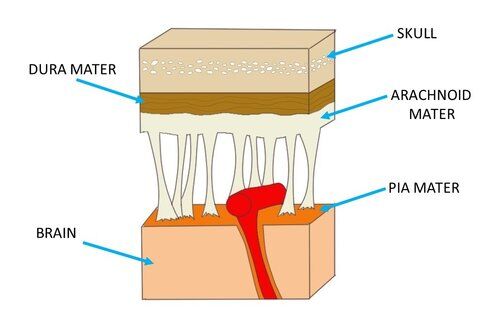
Introduction. The dura mater often gets referred to as merely the dura. It is one of the layers of connective tissue that make up the meninges of the brain (pia, arachnoid, and dura, from inside to outside). It is the outermost layer of the three meninges that surround and protect the brain and spinal cord.
The dura mater is a sac that envelops the arachnoid and has been modified to serve several functions. The dura mater surrounds and supports the large venous channels (dural sinuses) carrying blood from the brain toward the heart. The dura mater is partitioned into several septa, which support the brain.
Summary
The dura mater is a thick membranous sac, attached cranially around the greater foramen of the occiput, where its fibres blend with the inner periosteum of the skull, and anchored distally to the dorsal surface of the distal sacrum by the filum terminale. The latter descends to the coccyx, where its fibres merge with the connective tissue of the sacroiliac ligaments. The dural sac itself ends blind, usually at S2. There is an inconstant dural attachment, the ‘Hofmann complex’, made up of bands of connective tissue and loosely joining the anterior dura to the vertebral column. Ventral meningovertebral ligaments pass from the ventral surface of the dura to the posterior longitudinal ligament. They are variable in structure and may present either as tight bands, bifurcations in a Y shape or paramedian bands. Others reported on more lateral ligaments, passing from the lateral surface of the dural sac and blending with the periosteum of the pedicles.
At the lumbar level, the dura contains the distal end of the spinal cord (conus medullaris, ending at L1), the cauda equina and the spinal nerves, all floating and buffered in the cerebrospinal fluid. The lumbar roots have an intra- and extrathecal course. Emerging in pairs from the spinal cord, they pass freely through the subarachnoid space before leaving the dura mater. In their extrathecal course and down to the intervertebral foramen, they remain covered by a dural investment. At the L1 and L2 levels, the nerves exit from the dural sac almost at a right angle and pass across the lower border of the vertebra to reach the intervertebral foramen above the disc. From L2 downwards, the nerves leave the dura slightly more proximally than the foramen through which they will pass, thus having a more and more oblique direction and an increasing length within the spinal canal.
The dura mater has two characteristics that are of cardinal clinical importance: mobility and sensitivity.
Details
In neuroanatomy, dura mater is a thick membrane made of dense irregular connective tissue that surrounds the brain and spinal cord. It is the outermost of the three layers of membrane called the meninges that protect the central nervous system. The other two meningeal layers are the arachnoid mater and the pia mater. It envelops the arachnoid mater, which is responsible for keeping in the cerebrospinal fluid. It is derived primarily from the neural crest cell population, with postnatal contributions of the paraxial mesoderm.
Structure
The dura mater has several functions and layers. The dura mater is a membrane that envelops the arachnoid mater. It surrounds and supports the dural venous sinuses that reabsorbs cerebrospinal fluid and carries the cerebral venous return back toward the heart.
Cranial dura mater has two layers or lamellae, which include a superficial periosteal layer that is actually the inner periosteum of the neurocranium (the calvarium and endocranium); and a deep meningeal layer, which is the true dura mater. The dura mater covering the spinal cord is known as the dural sac or thecal sac, and only has one layer (the meningeal layer) unlike cranial dura mater. The potential space between these two layers is known as the epidural space, which can accumulate blood in the case of traumatic laceration to the meningeal arteries.
Folds and reflections
The dura separates into two layers at dural reflections (also known as dural folds), places where the inner dural layer is reflected as sheet-like protrusions into the cranial cavity. There are two main dural reflections:
* The tentorium cerebelli exists between and separates the cerebellum and brainstem from the occipital lobes of the cerebrum.
* The falx cerebri, which separates the two hemispheres of the brain, is located in the longitudinal cerebral fissure between the hemispheres.
Two other dural infoldings are the cerebellar falx and the sellar diaphragm:
* The cerebellar falx (falx cerebelli) is a vertical dural infolding that lies inferior to the cerebellar tentorium in the posterior part of the posterior cranial fossa. It partially separates the cerebellar hemispheres.
* The sellar diaphragm is the smallest dural infolding and is a circular sheet of dura that is suspended between the clinoid processes, forming a partial roof over the hypophysial fossa. The sellar diaphragm covers the pituitary gland in this fossa and has an aperture for passage of the infundibulum (pituitary stalk) and hypophysial veins.
Blood supply
This depends upon the area of the cranial cavity: in the anterior cranial fossa the anterior meningeal artery (branch from the ethmoidal artery) is responsible for blood supply, in the middle cranial fossa the middle meningeal artery and some accessory arteries are responsible for blood supply, the middle meningeal artery is a direct branch from the maxillary artery and enter the cranial cavity through the foramen spinosum and then divides into anterior (which runs usually in vertical direction across the pterion) and posterior (which runs posterosuperiorly) branches, while the accessory meningeal arteries (which are branches from the maxillary artery) enter the skull through foramen ovale and supply area between the two foramina, and the in posterior cranial fossa the dura mater has numerous blood supply from different possible arteries:
A. posterior meningeal artery (from the ascending pharyngeal artery through the jugular foramen)
B. meningeal arteries (from the ascending pharyngeal artery through hypoglossal canal)
C. meningeal arteries (from occipital artery through jugular or mastoid foramen)
D. meningeal arteries (from vertebral artery through foramen magnum)
Drainage
The two layers of dura mater run together throughout most of the skull. Where they separate, the gap between them is called a dural venous sinus. These sinuses drain blood and cerebrospinal fluid (CSF) from the brain and empty into the internal jugular vein.
Arachnoid villi, which are outgrowths of the arachnoid mater (the middle meningeal layer), extend into the dural venous sinuses to drain CSF. These villi act as one-way valves. Meningeal veins, which course through the dura mater, and bridging veins, which drain the underlying neural tissue and puncture the dura mater, empty into these dural sinuses. A rupture of a bridging vein causes a subdural hematoma.
Nerve supply
The supratentorial dura mater membrane is supplied by small meningeal branches of the trigeminal nerve (V1, V2 and V3). The innervation for the infratentorial dura mater are via upper cervical nerves and the meningeal branch of the vagus nerve.
Clinical significance
Many medical conditions involve the dura mater. A subdural hematoma occurs when there is an abnormal collection of blood between the dura and the arachnoid, usually as a result of torn bridging veins secondary to head trauma. An epidural hematoma is a collection of blood between the dura and the inner surface of the skull, and is usually due to arterial bleeding. Intradural procedures, such as removal of a brain tumour or treatment of trigeminal neuralgia via a microvascular decompression, require that an incision is made to the dura mater. To achieve a watertight repair and avoid potential post-operative complications, the dura is typically closed with sutures. If there is a dural deficiency, then a dural substitute may be used to replace this membrane. Small gaps in the dura can be covered with a surgical sealant film.
In 2011, researchers discovered a connective tissue bridge from the rectus capitis posterior major to the cervical dura mater. Various clinical manifestations may be linked to this anatomical relationship such as headaches, trigeminal neuralgia and other symptoms that involved the cervical dura. The rectus capitis posterior minor has a similar attachment.
The dura-muscular, dura-ligamentous connections in the upper cervical spine and occipital areas may provide anatomic and physiologic answers to the cause of the cervicogenic headache. This proposal would further explain manipulation's efficacy in the treatment of cervicogenic headache.
The American Red Cross and some other agencies accepting blood donations consider dura mater transplants, along with receipt of pituitary-derived growth hormone, a risk factor due to concerns about Creutzfeldt–Jakob disease.
Cerebellar tonsillar ectopia, or Chiari malformation, is a condition that was previously thought to be congenital but can be induced by trauma, particularly whiplash trauma. Dural strain may be pulling the cerebellum inferiorly, or skull distortions may be pushing the brain inferiorly.
Dural ectasia is the enlargement of the dura and is common in connective tissue disorders, such as Marfan syndrome and Ehlers–Danlos syndrome. These conditions are sometimes found in conjunction with Arnold–Chiari malformation.
Spontaneous cerebrospinal fluid leak is the fluid and pressure loss of spinal fluid due to holes in the dura mater.
It appears to me that if one wants to make progress in mathematics, one should study the masters and not the pupils. - Niels Henrik Abel.
Nothing is better than reading and gaining more and more knowledge - Stephen William Hawking.
Offline
Pages: 1